Long-term use of serotonin-based antidepressants can significantly impact the efficacy of psychedelic therapy, as both treatments interact with the brain’s serotonergic system.
Understanding the nuances of their interaction is crucial for individuals seeking relief from persistent mental health conditions through emerging modalities like psychedelic therapy.
In the ongoing evolution of mental health treatments, the integration of traditional pharmacotherapy, such as antidepressants, with emerging modalities like psychedelic therapy, presents both promising synergies and significant challenges.
The journey toward mental wellness is complex, with each individual presenting a unique constellation of symptoms, responses, and recovery paths. At the heart of this journey lies a critical component: the brain’s serotonergic system, a central player in mood regulation, psychological well-being, and the mechanism of action for both antidepressants and psychedelics.
This article delves into the intricate dance between the long-term use of serotonin-based antidepressants and the burgeoning field of psychedelic therapy, exploring the nuances of their interaction and the implications for individuals seeking relief from persistent mental health conditions.
Download Our Free Psilocybin Sourcing Guide
For harm-reduction purposes, we provide links to online psilocybin vendors, local stores, delivery services, and spore vendors for growing your own medicine at home.
Key Takeaways
-
- Antidepressant-Psychedelic Interaction: Long-term antidepressant use affects psychedelic therapy’s efficacy, emphasizing the need to understand their interaction within the serotonergic system.
-
- Transition Risks and Management: Switching from antidepressants to psychedelics requires careful management of withdrawal and serotonin syndrome risks, especially with MAOIs, highlighting the importance of a personalized washout period for safety.
-
- Influence on Therapy Outcomes: Changes in receptor density and neurotransmitter dynamics from chronic antidepressant use can impact psychedelic therapy’s effectiveness, suggesting adjustments in treatment plans may be necessary to leverage the benefits of psychedelics.
-
- Psychedelic Passage: Your Psychedelic Concierge — The easy, legal way to find trustworthy psilocybin guides, facilitators and psychedelic-assisted therapy near you in the United States.
Background on Antidepressant Mechanisms of Action
Antidepressants aim to correct the chemical imbalances in the brain associated with mood disorders. They achieve this by modulating the activity of neurotransmitters—chemical messengers such as serotonin, noradrenaline, and, to a lesser extent, dopamine.
By increasing the availability of these neurotransmitters in the synaptic cleft, antidepressants can alleviate the symptoms of depression and improve mood.
-
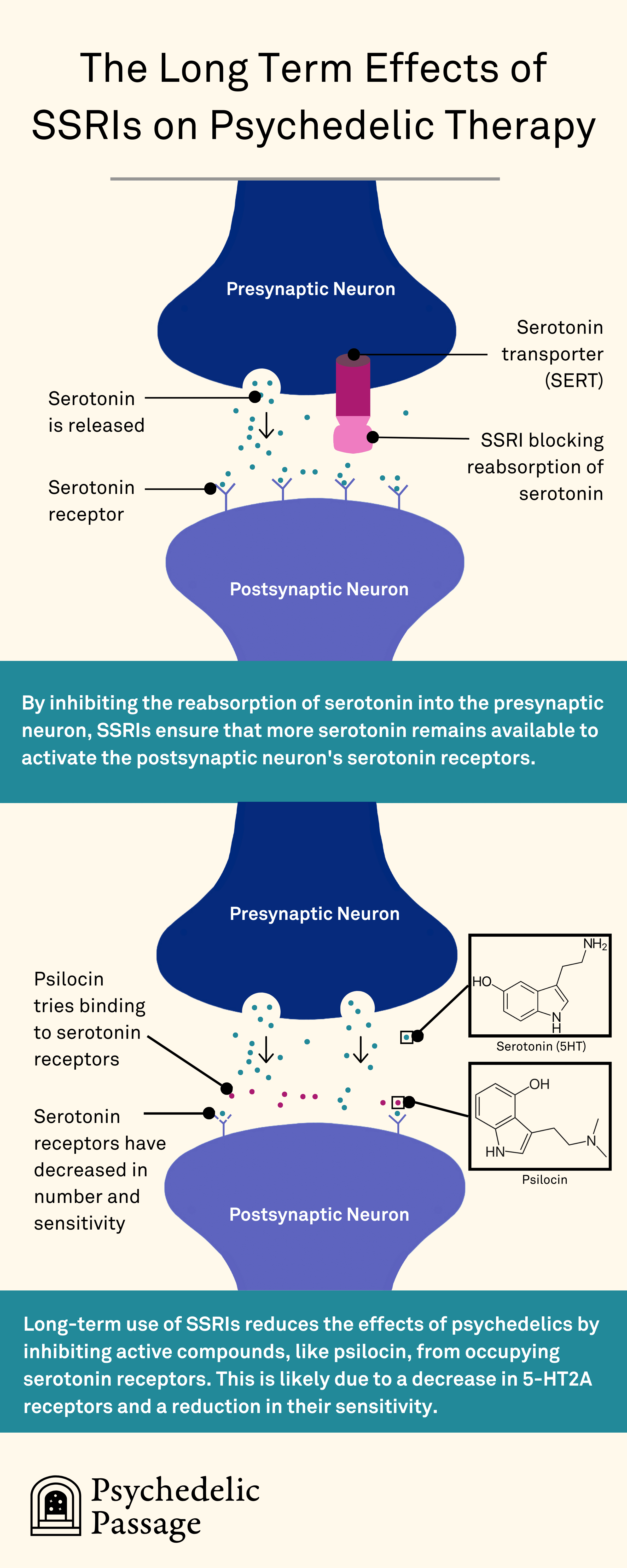
- SSRIs, or Selective Serotonin Reuptake Inhibitors, work by selectively blocking the reuptake of serotonin, increasing its concentration in the synaptic space and enhancing mood regulation.
-
- SNRIs, or Serotonin and Norepinephrine Reuptake Inhibitors, similarly increase serotonin levels but also target noradrenaline, offering a broader approach to mood improvement.
-
- NDRIs, or Norepinephrine-Dopamine Reuptake Inhibitors, function by blocking the reuptake of two key neurotransmitters in the brain: norepinephrine and dopamine.
-
- TCAs and MAOIs, or Tricyclic Antidepressants and Monoamine Oxidase Inhibitors, while less commonly used today due to their side effect profiles, operate through mechanisms that increase neurotransmitter levels by inhibiting their reuptake or breakdown.
Complete List of Antidepressant Medication Names
| Brand Name | Generic Name | Type |
| N/A (Formerly Elavil) | amitriptyline | Tricyclic |
| Wellbutrin, Zyban | bupropion | NDRI |
| Celexa | citalopram | SSRI |
| Pristiq, Khedezla | desvenlafaxine | SNRI |
| BuSpar | buspirone | Anxiolytic |
| Pamelor | doxepin | Tricyclic |
| Cymbalta | duloxetine | SNRI |
| Lexapro | escitalopram | SSRI |
| Prozac | fluoxetine | SSRI |
| Luvox | fluvoxamine | SSRI |
| Marplan | isocarboxazid | MAOI |
| Remeron | mirtazapine | Atypical |
| Pamelor | nortriptyline | Tricyclic |
| Paxil, Pexeva | paroxetine | SSRI |
| Nardil | phenelzine | MAOI |
| Emsam | selegiline | MAOI |
| Zoloft | sertraline | SSRI |
| Parnate | tranylcypromine | MAOI |
| Desyrel, Oleptro | trazodone | Atypical |
| Effexor | venlafaxine | SNRI |
| Viibryd | vilazodone | SSRI |
| Trintellix | vortioxetine | SSRI |
Long-term Effects of Antidepressant Use
Antidepressants, especially SSRIs, operate by inhibiting the reuptake of serotonin, a neurotransmitter pivotal in regulating mood, anxiety, and happiness. This mechanism increases serotonin availability in the synaptic space, theoretically ameliorating symptoms of depression and anxiety.
Chronic antidepressant use induces physiological changes beyond serotonin reuptake inhibition, including alterations in gene expression, receptor density, and neurotransmitter dynamics.
Despite their immediate action, the full benefits of SSRIs are usually seen after weeks or months, suggesting that other changes over time play a role in their effectiveness.
A study by Benmansour et al. (1999) used advanced techniques to measure how chronic use of SSRIs changes serotonin transporter (SERT) activity and levels in the brain, finding that SSRIs, but not other antidepressants, significantly downregulates SERT activity and levels.
SERT, a monoamine transporter protein, facilitates the reuptake of the neurotransmitter serotonin from the synaptic cleft into the presynaptic neuron, a mechanism referred to as serotonin reuptake.
Interestingly, the study found that the SNRI desipramine did not decrease SERT density, suggesting a unique action of SSRIs on serotonergic systems.
These findings are important for understanding why it might take a while for antidepressants to work and why some people might stop responding to treatment over time. As the SERT is the primary target of SSRIs, its reduction is a form of physiological adaptation which could diminish the effectiveness of these drugs, potentially necessitating adjustments in treatment strategies for certain patients.
These changes can have profound implications on neural plasticity, emotional regulation, and stress response systems. While some of these adaptations may be beneficial in the context of antidepressant efficacy, the reduced sensitivity and decrease of serotonin receptors over time renders the brain less responsive to serotonin mediated therapies, including psychedelics.
Recommended Reading: The Psilocybin-Blunting Effects of SSRIs and Antidepressants
Zhao et al.’s 2008 study confirms this assertion, finding that chronic treatment with certain antidepressants reduces the expression of norepinephrine transporters (NET) or SERT.
This downregulation was observed with SNRIs like protriptyline and reboxetine (for NET) and the SSRI sertraline (for SERT), but not with all antidepressants tested. For instance, venlafaxine, which inhibits both NET and SERT, produced antidepressant-like effects without altering transporter expression.
These findings may shed light on why, within our pre-vetted network of psychedelic facilitators, it’s observed that for some SSRIs, gradual reduction (tapering) is necessary to experience the effects of psychedelics. In contrast, for other SSRIs, increasing the dosage is often sufficient to feel their effects.
“Effexor I’ve never seen people journey on even after eating 10+ grams of Penis Envy, and on Lexapro people tend to have an experience without any tapering.”
– Facilitator in Psychedelic Passage network
Please note: The statement about Effexor and Lexapro’s interactions with psychedelics is based on anecdotal evidence and may not apply to everyone. Individual responses to medications and substances vary.
The Physiological Benefits of Psychedelic Therapy
Mental health treatment has heavily relied on SSRIs for mood and anxiety disorders due to their effectiveness for some. However, the notion that depression solely results from a serotonin deficit is being heavily questioned.
Recent consensus suggests SSRIs’ benefits may stem from their ability to enhance neuroplasticity, the brain’s ability to adapt and reorganize itself, rather than just boosting serotonin.
This neuroplasticity, often driven by growth factors like Brain-Derived Neurotrophic Factor (BDNF), unfolds over weeks, indicating the long-term impact of SSRIs beyond their immediate serotonergic effects.
Research highlights that psychedelics like psilocybin and LSD, known for their rapid and lasting antidepressant effects, also promote neuroplasticity through mechanisms similar to traditional antidepressants.
These substances bind directly to TrkB, the BDNF receptor, with much higher affinity than SSRIs, suggesting a significant and potentially more effective role in their antidepressant effects.
Insights like this have shifted the focus towards psychedelics and other treatments that leverage neuroplasticity for mental health, suggesting that strategies beyond traditional antidepressants, including therapy and lifestyle changes, could be more effective for treating depression.
The Impact of Long Term Antidepressant Use on Psychedelic Therapy
Psychedelic therapy, utilizing compounds like psilocybin, acts significantly on the same serotonin 2A receptors that SSRIs target, which are crucial for the therapeutic effects attributed to psychedelics, including enhanced neuroplasticity and profound changes in perception and self-awareness.
The downregulation of receptors induced by long-term antidepressant use poses a dilemma; it can blunt the effects of psychedelics, rendering them less effective or necessitating a pause in medication that can span weeks to allow for receptor recovery and serotonin regulation.
“The shortest tapering period reported by a client was 2 weeks, which involved a moderate dose of Lexapro. The longest tapering duration I have observed was 6 weeks, from a regimen of 50mg Pristiq and 100mg Fluvoxamine.
This extended period was primarily to ensure the client reached a stable emotional and mental state, with the actual tapering completed in 4 weeks, followed by an additional 2 weeks for assurance.
Additionally, the client was using 0.5 mg Xanax on an as-needed basis, approximately 2-4 times per month, and continued its use until a week before the ceremony.”
– Facilitator in Psychedelic Passage Network
Transitioning from Antidepressants to Psychedelic Therapy
Considerations for Discontinuing SSRIs & SNRIs and Starting Psychedelics
The discontinuation of SSRIs and SNRIs, often necessary for engaging in psychedelic therapy, can induce a withdrawal syndrome characterized by a spectrum of physical and psychological symptoms.
These symptoms can range from nausea and vertigo to more peculiar sensations like “brain zaps,” reflecting the body’s struggle to adapt to the sudden absence of the drug’s influence on serotonin levels.
This withdrawal phase can exacerbate the underlying conditions the SSRIs were prescribed to manage, presenting a paradox where individuals seeking healing from psychedelic therapy might face a temporary intensification of their symptoms prior to their psychedelic experience.
Thus, this transition period requires careful management to mitigate withdrawal effects and prepare the individual for psychedelic therapy.
Strategies such as tapering off antidepressants, implementing supportive therapies, and, in some cases, utilizing microdosing protocols, can provide a smoother transition and minimize the risk of exacerbating underlying conditions.
Recommended Reading: Should I Stop Using Antidepressants For Psychedelic Therapy?
Considerations for Discontinuing MAOIs and Starting Psychedelics
When it comes to managing depression, Monoamine Oxidase Inhibitors (MAOIs) have been a cornerstone of treatment. However, transitioning from MAOIs to other antidepressants or exploring the therapeutic potential of psychedelics like psilocybin and LSD requires caution due to the risk of serotonin syndrome (SS).
This potentially life-threatening condition arises from an excess of serotonin in the brain, leading to symptoms ranging from restlessness and sweating to severe hypertension and confusion.
A case reported in 2011 underscores the importance of a sufficient washout period when switching from MAOIs to other serotonergic medications. In this case, a patient experienced serotonin syndrome upon starting venlafaxine (SNRI) just two weeks after discontinuing phenelzine, an irreversible MAOI.
The symptoms, which included restlessness, shivering, elevated blood pressure, and tachycardia, were indicative of serotonin syndrome as defined by Sternbach’s criteria.
Serotonin syndrome is triggered by increased serotonin levels due to various mechanisms, such as inhibition of its metabolism by MAOIs, increased formation, or enhanced sensitivity of postsynaptic receptors.
The case highlights that even a 2-week washout period, commonly recommended when switching from MAOIs to SSRIs or SNRIs, may not be sufficient to prevent serotonin syndrome. This is because the biosynthesis of monoamine oxidase, which is irreversibly inactivated by MAOIs, takes time to return to normal levels.
Evidence suggests that even a 4-week washout period may be inadequate for some individuals, emphasizing the need for caution and close monitoring when introducing serotonergic drugs after MAOI discontinuation.
Like SSRIs and SNRIs, psychedelics can lead to increased serotonin levels, raising the risk of serotonin syndrome if used too soon after stopping MAOIs. Therefore, a careful washout period is necessary before the use of psychedelics to ensure safety and avoid adverse reactions.
Considerations for Discontinuing TCAs and Starting Psychedelics
The considerations for switching from TCAs to SSRIs, particularly fluoxetine, fluvoxamine, and paroxetine, shed light on the potential risks and precautions necessary when contemplating the use of psychedelics after TCAs.
Fluvoxamine, fluoxetine, and paroxetine are known for their inhibition of liver enzymes CYP1A2 and CYP2D6. These enzymes play a crucial role in the metabolism of TCAs, and their inhibition can lead to increased levels of TCAs in the body, potentially causing adverse effects.
Similar caution is warranted when considering the use of psychedelics such as LSD, which is also metabolized by these cytochrome P450 (CYP) isoforms. Research has shown that the functionality of CYP2D6, in particular, significantly influences the pharmacokinetics of LSD, affecting both the intensity and duration of its effects.
Individuals with inhibited or nonfunctional CYP2D6 due to the lingering influence of TCAs may experience heightened and prolonged psychedelic effects. This is an essential consideration for those looking to explore psychedelics for therapeutic purposes or personal exploration after being treated with TCAs.
Studies have confirmed this, finding that the chronic use of TCAs can amplify the hallucinatory effects of LSD, suggesting a significant interaction between TCAs and psychedelics.
Recommended Reading: Our Antidepressant and Psychedelic Drug Interaction & Taper Guide will teach you how to transition from antidepressants to psychedelic therapy, while buffering withdrawal symptoms, maintaining psychological stability, and gradually reintroducing the brain to the serotonergic activity, without overwhelming the system.
A Guide to Antidepressants and Psychedelic Therapy
Exploring the intersection of traditional pharmacotherapy and the emerging field of psychedelic therapy opens new avenues for understanding and treating mental health conditions. Delve deeper into this subject with our curated resources:
-
- Understanding Interactions: Learn about The Psilocybin-Blunting Effects of SSRIs and Antidepressants, providing essential insights into how conventional antidepressants might influence the efficacy of psilocybin and other psychedelics.
-
- Making Informed Decisions: Contemplating whether to pause or discontinue antidepressant medication in preparation for psychedelic therapy? Explore Should I Stop Using Antidepressants For Psychedelic Therapy? for guidance on navigating this complex decision.
-
- Insights from Experts: Listen to our podcast episode on SSRIs, Antidepressants, and Psilocybin, featuring discussions with our co-founders about the nuanced relationship between SSRIs, antidepressants, and the use of psilocybin.
-
- Expert Guidance on Tapering: Seeking advice on safely transitioning from antidepressants to engage in psychedelic therapy? Dr. Ben Malcolm, the Spirit Pharmacist, shares his expertise in Psychedelics, Antidepressants, & Tapering, offering strategies for tapering and mitigating withdrawal symptoms.
Find Confidence and Clarity with Psychedelic Passage’s Guidance
Hi there! We sincerely hope that you’ve found valuable takeaways that resonate with your current intentions. To explore research-based education, stay updated with psychedelic news, and benefit from practical how-to articles, we encourage you to head over to our resources page.
If you’re seeking personalized advice and are prepared to take the first step toward a therapeutic psychedelic experience, we invite you to book a consultation with our team of experienced psychedelic concierges.
This consultation is more than just a conversation; it’s an opportunity to be matched with a trustworthy local facilitator. You’ll be seamlessly connected to our rigorously vetted network of psychedelic guides, ensuring potential matches align with your needs.
Psychedelic Passage offers confidence and peace of mind by alleviating the burden of having to guess who’s right for you. If you want to discover how Psychedelic Passage can help you, we empower you to learn more about our services and check out client testimonials from those who’ve gone before you.
Your healing path is uniquely yours, and our commitment is to serve you at every juncture. Psychedelic Passage: Your Psychedelic Concierge — The easy, legal way to find trustworthy psilocybin guides, facilitators and psychedelic-assisted therapy near you in the United States.
Learn More About Our Network
Connect with Psychedelic Passage
-
- Listen to our podcast on Spotify, Apple Podcasts, and iHeartRadio
- Subscribe to our Youtube Channel
- Follow us on Instagram, Reddit, and Linked in for bite-sized updates and content.
Frequently Asked Questions: Antidepressant Use & Psychedelic Therapy
1. How do antidepressants and psychedelics interact within the brain’s serotonergic system?
Antidepressants, particularly SSRIs and SNRIs, increase the availability of neurotransmitters like serotonin in the brain, enhancing mood regulation.
Psychedelics act on the same serotonergic system, particularly targeting serotonin 2A receptors, to induce profound changes in perception and mood. Long-term antidepressant use can alter receptor density and neurotransmitter dynamics, often influencing the efficacy and experience of psychedelic therapy.
2. What are the potential risks of combining long-term antidepressant use with psychedelic therapy?
The main risk is the blunting of psychedelic effects due to the downregulation of serotonin receptors induced by chronic antidepressant use. This adaptation could make individuals less responsive to psychedelics, requiring a washout period before engaging in psychedelic therapy to avoid reduced effects or serotonin syndrome in cases involving MAOIs.
3. Can you switch directly from antidepressants to psychedelic therapy?
Direct switching is not recommended due to potential withdrawal symptoms from antidepressants and the risk of serotonin syndrome, especially with MAOIs.
A careful tapering of antidepressants, under medical supervision, is advised to minimize withdrawal effects and ensure safety during the transition to psychedelic therapy.
4. What is the recommended washout period when transitioning from MAOIs or TCAs to psychedelics?
For MAOIs, a washout period of more than two weeks, and possibly up to four weeks or longer, may be necessary to avoid serotonin syndrome. The exact duration depends on individual factors and the specific MAOI used.
For TCAs, caution is also advised due to their interaction with liver enzymes that metabolize psychedelics, affecting the psychedelic experience’s intensity and duration.
5. How does long-term use of antidepressants affect the therapeutic outcomes of psychedelic therapy?
Long-term antidepressant use can lead to physiological changes that potentially diminish the effectiveness of psychedelic therapy.
These include alterations in receptor density and neurotransmitter availability, which might necessitate a pause or adjustment in medication to allow the brain’s serotonergic system to recover and respond optimally to psychedelics.



